Microglia: A Role in Alzheimer’s Disease?
- P.K. Peterson

- Dec 4, 2024
- 4 min read
“Defining cell types is crucial for understanding new biological phenomena, elucidating underlying mechanisms, and identifying therapy targets.”
Zhang Zhang, PhD, bioinformaticist, Beijing Institute of Genomics, Chinese Academy of Sciences
“Society is entering an era in which the unchecked devastation of Alzheimer’s disease is no longer inevitable.”
Dennis Selkoe, MD, Alzheimer’s disease researcher, Harvard Medical School
Since 1906 when German clinical psychiatrist and neuroanatomist Alois Alzheimer first described it, Alzheimer’s disease (AD) has killed hundreds of millions of people. Currently, more people die of this cruel disease than breast and prostate cancer combined. And despite an extraordinary research effort, AD remains an idiopathic disease, that is nobody knows its cause, and a robust treatment has yet to materialize.
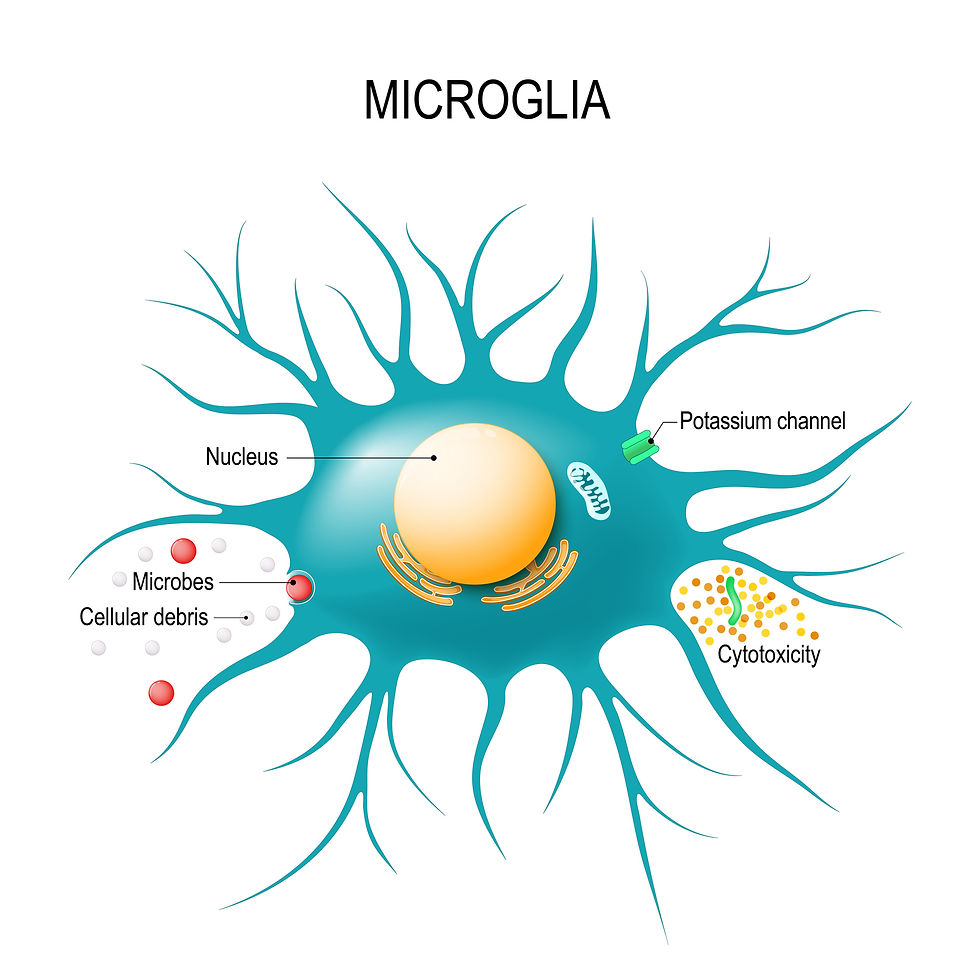
In today’s Germ Gems’ post, I feature brain cells called microglia, a type of immune cell that I fell in love with back in the day when my colleagues and I were trying to unravel the pathogenesis of brain damage caused by infectious agents. In addition, I introduce the concept that while microglia play a major role in defense of the brain, they may also behave like a “double-edged sword” and be involved in the neuropathogenesis of AD.

A simple-minded view of the brain. Several highly regarded scientists have described the human brain as “the most complex structure in the known universe.” Quite simply, however, the human brain is comprised of only two types of cells: neurons and glial cells. There are about as many non-neuronal cells (glial cells) as there are neurons (85 billion glia vs 86 billion neurons) in the human brain.
Neurons—the cells credited with your ability to think and move about—garner most of the attention of neuroscientists. In the October 24, 2024 issue of Nature, researchers described for the first time a map of every neuron in an animal’s (fruit fly’s) brain. The neuroscience research community hailed this extraordinary accomplishment.
But equally exciting to me was a September 2024 Nature publication from a multinational collaboration called the “Human Cell Atlas” that described the largest map of the human brain ever made. Behind this study was the deceptively simple question: what exactly is a cell type? According to neuroscientist Hongkui Zheng, director of the Allen Institute for Brain Science in Seattle, the answer is: “a group of cells that are similar to each other and distinct from other groups of cells.”
Many neuroscientists believe the best way to define a cell type is by the way it functions. For example, neurons are cells that generate thinking and our moving about. But what is the function of glial cells?
What do microglial cells do to and for the brain? The word glia comes from the ancient Greek word for “glue.” Scientists first recognized glial cells for their role in supporting neurons.
There are three major types of glia: microglia, astrocytes, and oligodendrocytes. Microglia captured most of the attention of researchers in our laboratory. While the name microglia suggest they are especially small, it’s only in comparison to the much larger astrocytes (or star-shaped cells) that microglia seem small.
Microglia constitute approximately 5-12% of the cells in the central nervous system—about 10 to 50 billion cells in all. First characterized in the 1910s by Pio del Rio-Hortega, a student of the Spanish neuroanatomist and founder of modern neuroscience, Santiago Ramon y Cajal, microglial cells are considered resident immune cells within the brain, where they function much as macrophages do throughout the body. In this capacity, they both fend off foreign invaders (pathogens) and “clean up the mess” that ensues with inflammation. And inflammation is regarded as a central mechanism in AD.
Within the context of their role in defending the brain, mounting evidence supports the causal role of a number of microbes in the pathogenesis of AD. (See “Is the Alzheimer Pandemic Caused by a Microbe?”, Germ Gems, February 23, 2021; “Hunt for infectious causes of Alzheimer’s gains momentum,” Research Gate, August 2, 2024).
In AD, it’s not only microbial pathogens that hypothetically can trigger neurodegeneration, but also a misfolded and aggregated protein called beta amyloid protein which forms sticky plaques in the brain that are a key pathological hallmark of AD. These plaques are believed to contribute to neuronal damage and cognitive decline associated with the disease.
In our neuroimmunology research laboratory, we demonstrated that beta amyloid protein induced injury of cultured human neurons and that a cytokine called transforming growth factor-beta protected neurons against beta-amyloid protein. (See “Transforming Growth Factor-B Protects Against B-Amyloid-Induced Injury,” Molecular and Chemical Neuropathology, 1994).
In the past decade, removal of or protection against beta amyloid protein plaques in AD has been the target of a large number of therapeutic trials. Most recently, a monoclonal antibody called lecanemab, developed by Biogen, that binds to toxic aggregates of beta-amyloid has been shown to produce significant reductions in cognitive decline in AD patients. As discussed in an August 2024 article in New Scientist, “How a new kind of vaccine could lead to the eradication of Alzheimer’s,” monoclonal antibodies are far from perfect, but those like lacanemab are opening a new frontier in the treatment of AD.

Harnessing the beneficent properties of microglia in the treatment of AD. Activated microglia can release neurotoxic mediators, like cytokines and free radicals, that may theoretically contribute to the pathogenesis of AD. Yet, when these brain macrophages find toxic material, such as beta amyloid protein coated with monoclonal antibodies, they may gobble up and neutralize its toxic activity. So, the dilemma is: how to involve only the beneficial side of the microglial cell double-edged sword in the battle against neurodegenerative diseases like AD?
For those suffering from devastating disorders like AD, progress in medical science often proceeds at a snail’s pace. Not uncommonly, when breakthroughs first arise from basic science research, they seem to have little practical value. And, although research on AD is advancing at an exciting pace, in my opinion more attention needs to be paid to microglia—the resident immune cells in the brain.
I’ve disclosed to several close friends and colleagues my opinion that neuroscientists—most of whom are in love with neurons—need to think of microglia not as “glue” but rather as master cells in the brain, directing many human behaviors now attributed to neurons, such as, eating, sleeping, and even enjoying music. (Would you believe Mozart is for your microglia?). I haven’t convinced any of them of the validity of this hypothesis. I only wish I would be around long enough to see a scientist thinking outside the box collect a Nobel Prize for providing convincing support of this hypothesis.




Comments